Project MARS: Multi-site Assessment of Risk for Suicide
- Adolescents
- Inpatients
- Wearables
- Smarphones
The goal of this study is to use smartphones and wearable physiological monitors to assess how and why negative life events affect adolescents’ risk for suicide.
Project Sleepio: Sleep treatment for Teens
- Intervention
- Adolescents
- Inpatients
- Wearables
- Smartphones
The purpose of this research study is to test a brief (6-session) version of digital cognitive behavioral therapy for insomnia (dCBT-I), called Sleepio in suicidal adolescents with co-occurring insomnia during the high-risk post-hospitalization period.
Project ADAPT: After-Discharge Assessment of Psychological skills Training
- Intervention
- Inpatients
- Smartphones
This study tests a telehealth adaptation of involving three brief skills training sessions during and after a suicidal individuals’ hospitalization followed by a smartphone-based ecological momentary intervention (EMI).
Project PUPS: Clarifying phenotypes of suicide risk in preteen youth
- Children
- Inpatients
- Wearables
The aim of this project will include an intensive process of adapting and refining an existing measure of suicidal thoughts, used in repeated-measures ecological momentary assessment studies (with multiple assessments per day) for preteens to be implemented in a daily diary format (a more developmentally appropriate and feasible design for this age and high-risk group which includes only one assessment per day).
E-Manage: Adaptive Evaluation of a Smartphone-Assisted Intervention for Emotion Management in College Students
- College Students
- Intervention
- Smartphones
The goal of this study is to test a treatment package consisting of a single-session intervention and companion smartphone app for college students experiencing distress.
Staff Opinions on Involuntary Hospitalization
- Providers
- Survey
- Burnout
This project will provide some of the very first information on the views of providers who treat individuals who are hospitalized involuntarily by surveying mental health workers or clinicians recruited from a multitude of hospitals across the country.
Project MARS: Multi-site Assessment of Risk for Suicide
MPI: Evan Kleiman, Cassie Glenn (Old Dominion University), and Richard Liu (Massachusetts General Hospital)
Locations: Rutgers University Behavioral Healthcare, Children’s Hospital of the King’s Daughters (Norfolk, VA), Massachusetts General Hospital (Boston, MA).
Funding: National Institute of Mental Health (R01MH124899)
Interpersonal negative life events (NLEs) such as conflict with friends and family have been consistently linked to short-term risk for suicidal behavior, but it is currently unclear how or why these events confer risk. Project MARS will examine the moderators and mechanisms linking interpersonal NLEs to suicidal behavior using an intensive real-time monitoring design. Specifically, we will ask 600 suicidal youth and their parents (recruited from three sites) to complete smartphone ecological momentary assessment and wearable actigraphy for the month after discharge from inpatient psychiatric care.
Project Sleepio: Sleep Treatment for Teens
MPI: Evan Kleiman and Cassie Glenn (Old Dominion University)
Locations: Rutgers University Behavioral Healthcare and Children’s Hospital of the King’s Daughters (Norfolk, VA)
Funding: National Institute of Mental Health (R34MH123590)

To reduce risk for STBs in youth, research identifying modifiable targets for intervention is greatly needed. Sleep problems, and particularly insomnia—the most common sleep problem in adolescents, may be one such promising treatment target. Insomnia has been consistently and uniquely linked to STBs (i.e., beyond depression), is associated with STBs over the short term (e.g., days, weeks), and is very treatable. Cognitive behavioral therapy for insomnia (CBT-I) is a brief (4-8 session) intervention with proven efficacy (medium-large effects) for reducing insomnia severity in adolescents and adults. In addition, CBT-I has been found to reduce a range of co-occurring psychiatric symptoms in adolescents (e.g., depression) and suicide ideation in adults.
The goal of Project Sleepio is to test a brief (6- session), empirically supported, and highly accessible version of dCBT-I, called Sleepio. This study will examine the feasibility and acceptability of delivering dCBT-I to suicidal adolescents with co-occurring insomnia during the post-hospitalization period, and examine the effectiveness of dCBT-I for reducing insomnia severity and suicide (STB) outcomes.
Project ADAPT: After-Discharge Assessment of Psychological Skills Training
MPI: Evan Kleiman and Kate Bentley (Massachusetts General Hospital)
Locations: Rutgers University Behavioral Healthcare and Brigham and Women’s Faulkner Hospital (Boston, MA)
Funding: National Institute of Mental Health (R34MH113757)

Though a number of in-person psychotherapy protocols have been developed or modified to address STBs, some of which have shown promising results, many individuals in need are unable to access such treatments. Barriers to accessing face-to-face psychotherapy include cost, difficulties with scheduling, distance from qualified providers, long waitlists, and perceived stigma. Telehealth, which facilitates delivery of evidence-based therapeutic content over videoconferencing technology or telephone sessions, may help overcome the barriers to accessing treatment and thus help suicidal individuals receive the care they need, including during particularly high-risk time periods.
This study proposes a telehealth adaptation of the intervention already tested by the Kleiman Lab which involves three brief in-person skills training sessions during suicidal individuals’ inpatient stays followed by a smartphone-based ecological momentary intervention (EMI). This study evaluates delivery of in-person skills training sessions over telehealth in two ways: (1) as a supplement to the in-person session(s) that participants are able to receive before being discharged, and (2) as a standalone intervention in which participants receive all three sessions via telehealth after discharge.
Project PUPS: Clarifying phenotypes of suicide risk in preteen youth
MPI: Evan Kleiman, Cassie Glenn (Old Dominion University), and Richard Liu (Massachusetts General Hospital)
Locations: Rutgers University Behavioral Healthcare, Children’s Hospital of the King’s Daughters (Norfolk, VA), Massachusetts General Hospital (Boston, MA).
Funding: National Institute of Mental Health (R01MH137793)
Suicide risk is increasing in preteens, 8-12 years old. Although research is limited, it is estimated that 15% of preteens in community samples and 43% in clinical samples have thought about suicide, and 3% in community and 18% in clinical samples of preteens have attempted suicide. Alarmingly, other than prevalence rates, we know very little about suicide risk in preteens. Specifically, we have limited understanding of key risk factors related to suicidal thoughts and behaviors in this age group. Our knowledge of suicide risk has been limited by the paucity of developmentally appropriate tools to assess suicidal thoughts, and relevant risk factors, in preteens.
Project PUPS seeks to adapt and validate a time-varying measure of suicide risk for preteens by conducting interviews with preteens and parents and receiving feedback about the assessment of suicidal thoughts, suicidal behaviors, and candidate risk factors for preteens. Then we will conduct a 28-day intensive longitudinal monitoring study with preteen/parent dyads to establish phenotypes of suicide risk consisting of self-reported risk, as well as objectively measured factors like sleep disturbance, acquired from a wrist worn biosensor. Finally, we seek to understand how these phenotypes predict risk for suicidal thoughts, suicidal behaviors, and other suicide-related events (e.g., rehospitalizations) across a 6-month follow-up.
E-Manage: Adaptive Evaluation of a Smartphone-Assisted Intervention for Emotion Management in College Students
MPI: Evan Kleiman and Kate Bentley (Massachusetts General Hospital)
Locations: Rutgers University – New Brunswick
Funding: National Institute of Mental Health (R01MH133191)
Rates of psychopathology in college students have risen, with nearly half of students now screening positive for anxiety or depression. This results in staggering demand on college counseling centers, many of which fall short of recommended student to therapist ratios. There is a need for scalable approaches to meeting the mental health needs of students, many of whom may not require weeks of resource-intensive 1:1 treatment.
E-Manage is a pilot study testing a multi-component psychological intervention that teaches college students key cognitive-behavioral skills for managing emotional distress. College students participate in a 90-minute workshop where they learning three skills derived from the Unified Protocol (UP) followed by completing 4 weeks of an ecological momentary intervention (EMI) where they were prompted to practice the skills that they learned from the workshop. The pilot will inform the Kleiman Lab’s future research on designing a Sequential Multiple Assignment Randomized Trial (SMART) to evaluate the effectiveness of this evidence-based intervention.
Staff Opinions on Involuntary Hospitalization
Involuntary hospitalization (also called involuntary commitment or civil commitment) is a legal process through which an individual with symptoms of severe mental disorder is detained in a psychiatric hospital (typically as an inpatient where they can be treated against their wishes. Involuntary hospitalization is often viewed as an experience that can have mixed impacts on the patients—ranging from positive (e.g., the patient is kept safe) to negative (e.g., stigma, cost to the patient).
This project: 1) characterizes how providers view their role in involuntary hospitalizations, 2) examines differences on providers’ views of involuntary hospitalization by relevant characteristics (e.g., years of training, years of experience, 3) examines the relationship between views of involuntary hospitalization and stigma towards mental illness, and 4) examines the relationship between involuntary hospitalization and provider burnount.
Past and Recently Completed Projects
Real-time intervention for reducing suicide risk
- Intervention
- Inpatients
- Wearables
- Smartphones
The goal of this study is to test an intervention delivery method that uses ecological momentary intervention (EMI) and wearable physiological monitoring to deliver a transdiagnostic, emotion-focused cognitive-behavioral therapy.
Real-time physiological assessment of emotion regulation as a mechanism of efficacy in Dialectical Behavior Therapy
- Intervention
- Outpatients
- Smartphones
- Wearables
The goal of this study is to observe how Dialectical Behavior Therapy (DBT), works to address emotion regulation, in real time, as emotion regulation actually occurs.
Evaluation of a brief, telehealth intervention to support emotional distress of autistic adults during COVID-19
- Intervention
- Outpatients
- Smartphones
This project aims to evaluate the utility of a new, brief, cost-effective treatment, the Emotional Support Plan (ESP), to help promote coping during periods of acute distress.
Pilot Study of a Brief, Scaleable Intervention for COVID-19 Mental Health Sequelae in College Students
- Intervention
- Smartphones
The major aim of this pilot study is to evaluate a brief coping skills intervention for college students, based on an evidence-based treatment and delivered remotely via 14 short videos.
A qualitative study of suicide risk assessment in smartphone studies
- Adolescents
- Inpatients
The goal of this study is to collect information using qualitative interviewing from suicidal adolescents and their parents, so that we can design an intervention protocol that considers the wishes, needs and perspective of those with lived experience and their caretakers.
Using ambulatory physiological monitoring to improve detection of harmful behaviors
- Adolescents
- Inpatients
- Wearables
The goal of this study will be to use physiological signals to detect psychological distress and the harmful behaviors that distress leads to in adolescent psychiatric inpatients as early as possible.
Real-time intervention for reducing suicide risk
PI: Evan Kleiman
Collaborators: Matt Nock (Harvard University) and Kate Bentley & Jeff Huffman (Massachusetts General Hospital/Harvard Medical School)
Location: Massachusetts General Hospital (Boston, MA) and Rutgers University Behavioral Healthcare (Piscataway, NJ)
Funding: National Institute of Mental Health (R34MH113757-01A1)

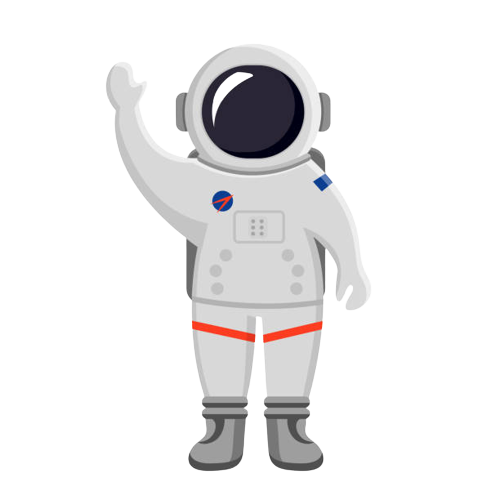
The time leading up to and during the experience of suicidal thoughts can be distressing. During a distressing “suicide crisis” it may be difficult for patients to access and use the skills they have learned in therapy. This lack of accessibility during the time when an intervention is most needed may be one reason why existing interventions are not as effective as they could be. Thus, interventions that are accessible and effective during a suicide crisis are needed. The goal of this study is to test an innovative intervention delivery method that uses two new technologies, ecological momentary intervention (EMI) and wearable physiological monitoring to deliver a transdiagnostic, emotion-focused cognitive-behavioral therapy.
The next step in this project is to create a Just-In-Time Adaptive Intervention (JITAI) where delivery of this brief intervention will happen not just at certain times or when triggered by the patient, but also in response to physiological changes that signal intense distress (e.g., changes in electrodermal activity over a short time period). Triggering interventions based on physiological signals of distress will make these interventions available just-in-time when they are needed with minimal input from the patient.
Real-time physiological assessment of emotion regulation as a mechanism of efficacy in Dialectical Behavior Therapy
Co-PIs: Shireen Rizvi and Evan Kleiman
Location:Dialectical Behavior Therapy Clinic at Rutgers University (DBT-RU)
Funding: Busch Biomedical Grant
Although effective treatments for suicide risk exist, such as Dialectical Behavior Therapy (DBT), we know little about how those treatments work. Such knowledge is critical for improving treatment efficacy and efficiency and making an impact on rates of suicide. An underlying theory of DBT is that individuals engage in NSSI or have suicidal thoughts as a means of regulating intense emotions to make these emotions more tolerable or socially acceptable. These methods serve to regulate emotion but do so at a cost of potential physical harm or increased risk for suicide in the future. Thus, it is hypothesized that DBT may work by targeting improvements in emotion regulation. This well-articulated hypothesis has not been tested because until recently, it has been difficult to assess emotion regulation in the most appropriate way. Emotion regulation occurs “in the moment” and thus people often have difficulty retrospectively reporting on whether or not they have engaged in emotion regulation. In this study, we will assess changes in emotion as these changes actually occur, using two novel technologies (smartphone-based ecological momentary assessment and wearable physiological monitoring) among a group of 20 adults who are undergoing DBT.
Evaluation of a brief, telehealth intervention to support emotional distress of autistic adults during COVID-19
Co-PIs: Vanessa Bal and Evan Kleiman
Funding: Rutgers Center for COVID-19 Response and Pandemic Preparedness (CCRP2)
Autistic adults are at high risk for depression, anxiety, and other mood dysregulation. Yet, there is a dearth of interventions to support their mental health needs. In particular, there are no empirically validated, brief interventions to support autistic adults in coping with acute emotional distress. The COVID-19 pandemic has amplified the dire need for brief, low-cost interventions that can be delivered via telehealth to support autistic adults to cope with their distress. Symptoms associated with autism, such as behavioral rigidity, inflexible adherence to routines and resistance to minor changes in daily life, coupled with impaired emotional regulation and fewer social supports, leave many autistic adults struggling to adapt to changes as unpredictable and drastic as those posed by the COVID-19 pandemic. With social distancing orders, many adults have lost their primary source of daily structure and support. Even as social distancing is relaxed, this population is likely to experience high levels of distress at yet another transition back to “normal”.
This project aims to evaluate the utility of a new, brief, cost-effective treatment, the Emotional Support Plan (ESP), to help promote coping during periods of acute distress. The driving concept behind this intervention is that ESPs will provide autistic adults with the necessary support to effectively manage distress. This study will provide an essential service to autistic adults during a time of crisis, as well as yield preliminary data to apply for extramural grants to validate these methods to monitor and support mental health of autistic adults during key transitions (e.g., starting college). Although the ESP intervention will support the immediate clinical needs of autistic adults during the COVID-19 pandemic, this intervention will have broad applicability to support emotion regulation and distress management far beyond the COVID-19 crisis.
Pilot Study of a Brief, Scaleable Intervention for COVID-19 Mental Health Sequelae in College Students
Co-PIs: Shireen Rizvi and Evan Kleiman
Funding: Rutgers Center for COVID-19 Response and Pandemic Preparedness (CCRP2)
College students are at high risk for mental health problems (e.g., anxiety, depression, substance use, suicidal thoughts/behaviors). The COVID-19 pandemic places them in a more dire situation. College counseling centers, already stretched with long waiting lists, are unlikely to meet the new demand. Resources must be devoted to alternatives to standard, resource-intensive mental health services. The major aim of this pilot study is to evaluate a brief coping skills intervention for college students, based on an evidence-based treatment and delivered remotely via 14 short videos.

A qualitative study of suicide risk assessment in smartphone studies
PI: Evan Kleiman
Collaborators: Matt Nock and Alex Millner (Harvard University) and Franciscan Children’s Hospital Mental Health Research Team
Location: Harvard University (Cambridge, MA) and Franciscan Children’s Hospital (Brighton, MA)
Funding: National Institute of Mental Health (R21MH115293-01S1)
Smartphone-based ecological momentary assessment (EMA) provides an unprecedented opportunity to capture fine grained assessments of suicidal thoughts and behaviors as they occur. These new technologies also bring unprecedented ethical, legal, methodological, and clinical concerns regarding participant safety. Specifically, having in situ data about urges to harm the self or others (especially in tandem with location data), raises the question how do we respond when a participant reveals that they are highly suicidal? The goal of this study is to collect information using qualitative interviewing from two key stakeholders, suicidal adolescents and their parents, so that we can design an intervention protocol that considers the wishes, needs and perspective of those with lived experience and their caretakers.
Using ambulatory physiological monitoring to improve detection of harmful behaviors
PI: Evan Kleiman
Collaborators: Matt Nock (Harvard University) and Franciscan Children’s Hospital Mental Health Research Team
Location: Franciscan Children’s Hospital (Brighton, MA)
Funding: National Institute of Mental Health (1R21MH115293)
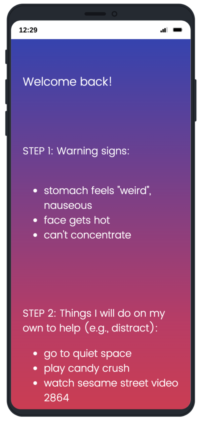
 Harmful behaviors (e.g., harm to self or others) resulting from rapidly increasing distress are unfortunately common experiences on adolescent inpatient units and often lead to interventions like seclusion, rather than more proactive methods that might have been effective before the distress escalated. The goal of this study is to use wearable physiological monitors to identify the early stages of distress that lead to harmful behaviors, which is not easily detectable by direct observation alone. We will collect data from these sensors and then match these data up to data already collected on the unit (e.g., checks sheet, data from EMR) to see how far before events like harm to self or others the physiological signs of distress are apparent.
Harmful behaviors (e.g., harm to self or others) resulting from rapidly increasing distress are unfortunately common experiences on adolescent inpatient units and often lead to interventions like seclusion, rather than more proactive methods that might have been effective before the distress escalated. The goal of this study is to use wearable physiological monitors to identify the early stages of distress that lead to harmful behaviors, which is not easily detectable by direct observation alone. We will collect data from these sensors and then match these data up to data already collected on the unit (e.g., checks sheet, data from EMR) to see how far before events like harm to self or others the physiological signs of distress are apparent.
This study will serve as the first step in creating a collaborative decision-making tool that can detect distress before it escalates to a harmful behavior, alerting clinical staff (e.g., on an iPad) to windows of time where more proactive interventions may be most likely to be effective.